A 55 year old male with SOB and pedal edema.
July 17 , 2023 CASE SHEET
CHIEF COMPLAINTS:
A 55 year old male patient resident of madhavagudem came to OPD with chief complaints
-SOB since 15 days
-pedal edema since 1 week
HOPI:
Patient was apparently asymptomatic 15days back then he developed SOB (grade 1and2) that was insidious in onset, gradually progressive
C/o pedal edema since 5 years and aggravated since last 15 days it is a pitting type
C/o decreased urine output since 1week
No C/O chest pain, palpitations, orthopnea, PND.
No H/O fever, burning micturition, loose stools, vomiting.
No C/O pain abdomen.
PAST HISTORY:
N/K/C/O HTN,DM epilepsy , TB ,thyroid disorder
K/C/O CKD diagnosed 1month back
PERSONAL HISTORY:
Diet - Mixed
Appatite - Normal
Sleep - Reduced
Bowel and Bladder - Reduced urination, normal bowel.
Allergy - None
Addictions
- Alcohol - about 90ml per day since his teenage.
- Bedi - 1 packet per day since his teenage.
FAMILY HISTORY:
No significant family history
GENERAL EXAMINATION:
The patient is conscious,coherent and cooperative; well oriented to time,place and person.
He is moderately build and well nourished.
Pallor - present
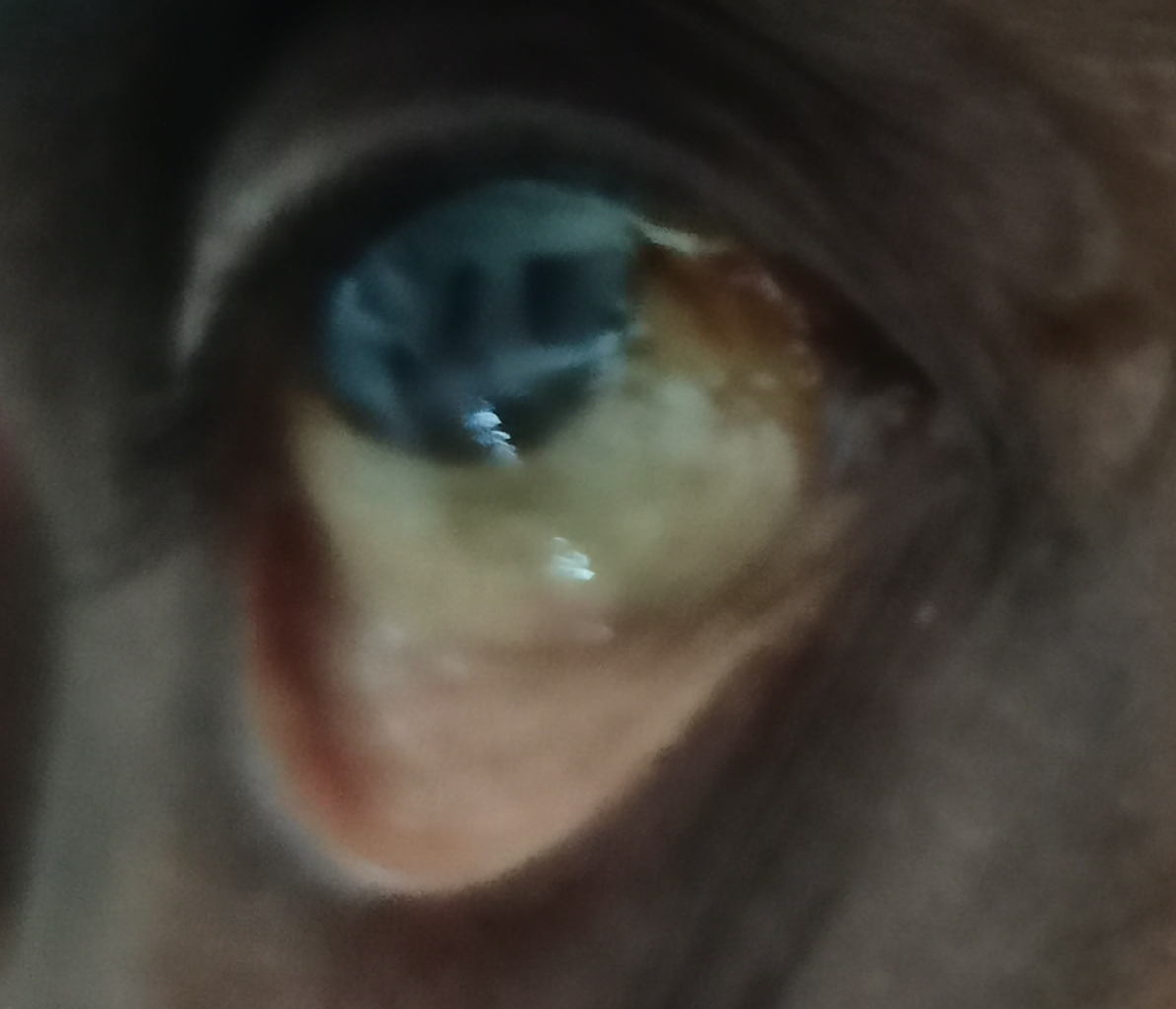
Icterus- present
Clubbing-absent
Cyanosis-absent
Lymphadenopathy-absent
Edema - B/L pitting type present, extending upto the knee.
Vitals:
Temperature -98.6F
Pulse rate - 94/ minute
Respiratory rate - 20/minute
Blood pressure (left arm) - 100/60 mm of Hg
GRBS - 105 mg/dl
Systemic Examination
Cardiovascular System-
- no thrills
- cardiac sounds S1 and S2 heard
- no cardiac murmurs
Respiratory System
no dyspnea
No wheezing
central trachea
vesicular breath sounds
Abdomen
Scaphoid shaped abdomen
No tenderness
No palpable mass
Non palpable liver and spleen
Bowel sounds -yes
CNS
Patient was conscious
Normal speech
INVESTIGATIONS :
ECG:









Comments
Post a Comment